If you’re allergic to bee pollen, you’re not alone. In recent years, there has been a significant rise in cases of this often-overlooked allergy. But what exactly is bee pollen allergy, and why should you be concerned? Simply put, an allergy to bee pollen occurs when your immune system overreacts to the protein-rich particles collected by bees from flowers. This can lead to a range of uncomfortable symptoms, from mild hives and itching to life-threatening anaphylaxis in severe cases. In this article, we’ll delve into the dangers of bee pollen allergy, its common symptoms, diagnosis methods, and most importantly, effective prevention strategies to minimize your risk. By understanding the risks associated with bee pollen allergy, you can take proactive steps to protect yourself and enjoy the outdoors without worry.
Risks Associated with Bee Pollen Consumption
While bee pollen can be a nutritious supplement, there are potential risks associated with its consumption that you should know about before adding it to your diet. Some of these risks may surprise you.
Common Symptoms of a Bee Pollen Allergy
If you’re allergic to bee pollen, it’s essential to recognize the common symptoms that can range from mild to severe. Skin reactions are often one of the first signs, manifesting as hives, itching, or redness. These skin issues may appear on any part of the body and can be quite uncomfortable.
Respiratory problems are another frequent symptom of a bee pollen allergy. This may include congestion, sneezing, runny nose, or even asthma-like symptoms. In severe cases, anaphylaxis can occur, which requires immediate medical attention. This life-threatening reaction can cause difficulty breathing, rapid heartbeat, and swelling of the face.
Gastrointestinal issues are also a common complaint among those with a bee pollen allergy. These may include stomach cramps, nausea, vomiting, or diarrhea. If you experience any of these symptoms after consuming bee pollen, it’s crucial to seek medical attention promptly.
Identifying High-Risk Individuals for Bee Pollen Allergies
When it comes to identifying high-risk individuals for bee pollen allergies, certain groups stand out due to their increased susceptibility. Children, pregnant women, and people with pre-existing allergies are among the most vulnerable.
Children’s immune systems are still developing, making them more prone to allergic reactions. If a child has a family history of allergies or has already shown signs of sensitivity to other allergens, it’s essential for parents to exercise caution when introducing bee pollen into their diet.
Pregnant women should also be cautious due to the potential impact on fetal development. Research suggests that exposure to environmental allergens during pregnancy may increase the risk of allergy in offspring.
If you fall into one of these categories or have a pre-existing allergy, it’s crucial to approach bee pollen consumption with caution. Start by introducing small amounts and monitor your body’s response. If symptoms persist or worsen, discontinue use immediately and consult a healthcare professional for guidance. By being aware of these risks and taking preventative measures, you can minimize the likelihood of developing a bee pollen allergy.
Causes of Bee Pollen Allergy Risk
One common question is, what causes bee pollen allergy risk? Let’s break down some of the key factors that contribute to developing an allergy.
Cross-Reactivity with Other Pollens
When you’re allergic to bee pollen, it’s not just that specific type of pollen that can trigger an issue. Your body may also react to other types of pollens, a phenomenon known as cross-reactivity. This is because many allergenic proteins found in different plant species share similar structures and are recognized by the immune system in a similar way.
For instance, if you’re allergic to ragweed pollen, you might find that grass pollen or even certain trees trigger a reaction due to their similarities in protein composition. Conversely, if you’re sensitive to cedar pollen, exposure to birch or alder may cause an issue as well. This is why it’s crucial to identify and monitor your specific allergenic triggers.
To manage cross-reactivity effectively, consider the following tips: Consult with your healthcare provider about the potential for cross-reactivity based on your specific allergy profile. If you have a known tree pollen allergy, take steps to minimize exposure during peak grass pollen seasons when ragweed is also present. By understanding how different pollens interact and working closely with your healthcare team, you can develop effective strategies for mitigating symptoms and avoiding severe reactions.
The Role of Genetic Predisposition
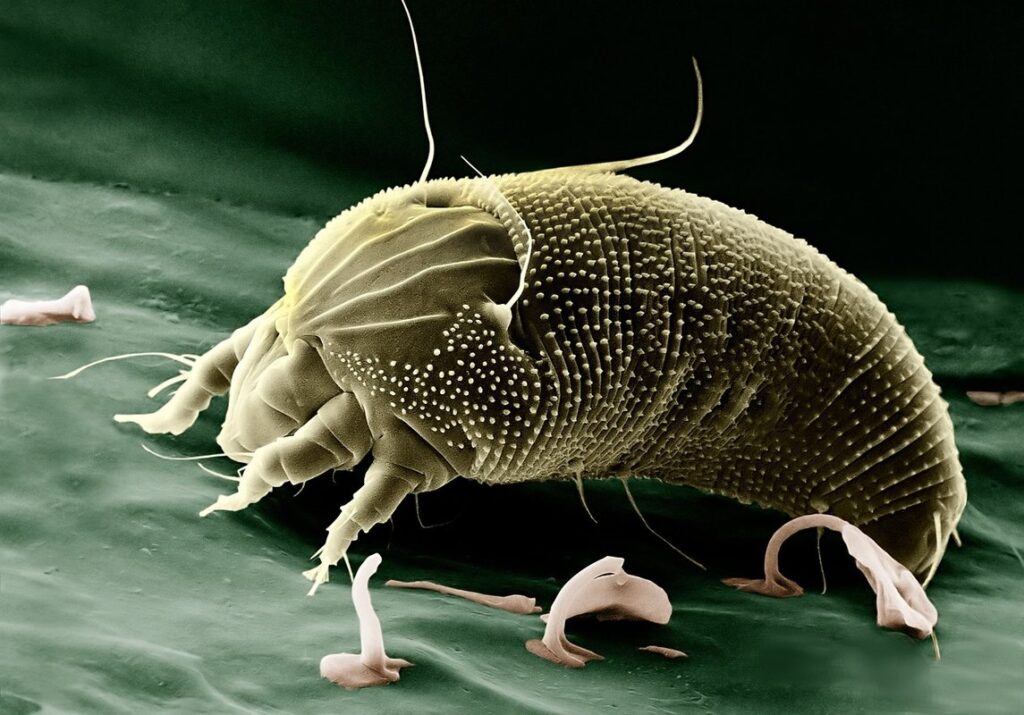
If you have a family history of allergies, particularly to bee pollen, dust mites, mold, pet dander, and other common allergens, it’s essential to be aware that your risk is higher. Research has shown that people with a genetic predisposition to allergies are more likely to develop sensitivities to various substances, including bee pollen.
Studies have found that individuals with a family history of allergies are 2-4 times more likely to develop an allergy themselves. This is because the tendency towards allergic reactions can be inherited from parents or grandparents through specific genes. If you’re aware of any allergies in your immediate or extended family, take note – it may influence your bee pollen allergy risk.
It’s not just about having a parent with allergies; even if both parents have allergies, the likelihood of their child developing an allergy increases significantly. Understanding your genetic predisposition can help you take preventive measures and make informed decisions about your exposure to potential allergens, including bee pollen.
Symptoms of a Bee Pollen Allergy
If you’re experiencing symptoms after consuming bee pollen, it’s essential to recognize the warning signs that indicate an allergy. This may include hives, itching, swelling, and digestive issues.
Skin Reactions and Rashes
If you’re allergic to bee pollen, it’s not just a matter of sneezing or sniffles – skin reactions can be some of the most uncomfortable and distressing symptoms. One of the most common skin issues associated with bee pollen allergy is hives. These itchy, red welts can appear anywhere on your body and are often accompanied by swelling. Imagine waking up to find large, raised patches on your arms or legs – not a pleasant way to start the day.
Another skin reaction that’s all too familiar for those with bee pollen allergy is eczema-like rashes. These dry, scaly patches can be incredibly itchy and may crack if scratched excessively. If you notice any changes in your skin after consuming bee pollen products or being exposed to bees, it’s essential to take note of the timing and severity of the reaction.
To manage these skin symptoms, keep an ice pack on hand to reduce swelling and itching. Antihistamines can also provide quick relief from hives and rashes. If you experience severe reactions or frequent occurrences, consult with your healthcare provider about long-term management options, such as allergy shots.
Respiratory Issues: Wheezing and Congestion
When you have a bee pollen allergy, it’s not just about skin rashes and itching – respiratory issues can also be a major concern. Wheezing, shortness of breath, and nasal congestion are common symptoms that can significantly impact daily life.
Wheezing is often the first sign of an oncoming asthma attack or allergic reaction. It sounds like a high-pitched whistling noise when you breathe out. This symptom can be particularly distressing if it’s your child who’s experiencing it. In such cases, monitor their breathing closely and seek medical attention immediately.
Nasal congestion is another respiratory issue associated with bee pollen allergy. Your nose may feel stuffy or blocked due to the release of histamine in response to an allergic reaction. This can make breathing through the nose difficult and lead to mouth breathing instead, which can cause a range of issues, including dry lips and throat irritation.
If you suspect that your symptoms are related to a bee pollen allergy, consult with your doctor for proper diagnosis and treatment. In the meantime, be sure to carry an EpiPen or other emergency medication with you at all times.
Diagnosing Bee Pollen Allergies
If you suspect you have a bee pollen allergy, it’s essential to identify the symptoms and determine the severity of your reaction. This section will guide you through the diagnosis process.
Blood Tests and Skin Prick Tests
When it comes to diagnosing a bee pollen allergy, there are two primary methods that doctors use: blood tests and skin prick tests. Both of these methods can provide valuable information about whether you have an allergic reaction to bee pollen.
Blood tests, such as RAST (RadioAllergoSorbent Test), measure the levels of IgE antibodies in your blood. These antibodies are produced by your immune system in response to exposure to a specific allergen, including bee pollen. A positive result means that you have IgE antibodies against bee pollen, which suggests an allergy.
A skin prick test is another common method for diagnosing allergies. During the test, a small amount of bee pollen extract is placed on your skin, and then a scratch or prick is made through it. If you’re allergic to bee pollen, a raised red bump will appear at the site within 15-20 minutes.
Both methods are reliable and accurate, but they may produce different results. Your doctor may use one or both of these tests to determine if you have an allergy to bee pollen.
Other Diagnostic Methods
In addition to skin prick tests and blood tests, other diagnostic methods can also help identify bee pollen allergies. One such method is a food challenge test, where a small amount of bee pollen is administered orally under medical supervision to assess the body’s reaction. This test is often used when other tests have produced inconclusive results.
Another method is an elimination diet, which involves removing all sources of bee pollen from the diet for a period of time and then reintroducing it to see if symptoms return. While this method can be effective, it requires careful monitoring and should only be attempted under the guidance of a healthcare professional.
In some cases, a doctor may also use a combination of diagnostic methods to confirm a diagnosis. For example, a patient with symptoms consistent with an allergy but inconclusive test results might undergo additional testing or observation to rule out other conditions.
Prevention Strategies for Bee Pollen Allergy
If you’re looking to minimize your risk of a bee pollen allergy, understanding effective prevention strategies is crucial. Here we’ll explore some practical ways to reduce exposure and alleviate symptoms.
Choosing Alternatives to Bee Pollen Supplements
If you’ve been diagnosed with a bee pollen allergy or are at risk of developing one, it’s essential to explore alternative supplements that can provide similar benefits without the risks. One option is green superfood powder, which is made from a blend of nutrient-rich algae and plants. This supplement offers many of the same health benefits as bee pollen, including high levels of antioxidants, vitamins, and minerals.
Another alternative is turmeric powder or capsules, which contain curcumin – a potent anti-inflammatory compound that has been shown to have numerous health benefits. Some studies suggest that taking turmeric daily can reduce inflammation and improve symptoms in individuals with allergies.
Consider trying spirulina supplements as well, which are derived from algae and packed with protein, iron, and other essential nutrients. Spirulina is rich in antioxidants and has anti-inflammatory properties, making it a great alternative to bee pollen for those with allergies.
When selecting an alternative supplement, be sure to read labels carefully and look for products that have been third-party tested for purity and potency. Additionally, consider consulting with a healthcare professional before introducing any new supplements into your diet.
Some popular alternatives to bee pollen include:
* Green superfood powder blends
* Turmeric capsules or powder
* Spirulina tablets or powder
* Chlorella supplements (made from algae)
When choosing an alternative supplement, prioritize products that are made from natural sources and have a good reputation for purity and effectiveness.
Managing an Existing Bee Pollen Allergy
If you’re already allergic to bee pollen, it’s crucial to take steps to minimize exposure and symptoms. This section will guide you on how to manage your existing allergy safely.
Lifestyle Changes and Avoidance Techniques
When managing an existing bee pollen allergy, it’s crucial to adopt lifestyle changes and avoidance techniques to minimize exposure. Start by making dietary adjustments – if you’re allergic to bee pollen, it’s likely that foods containing pollen will trigger a reaction. Common culprits include honey, apple sauce, and fruit juices. Be mindful of labels when shopping for packaged goods, as many products may contain pollen-derived ingredients.
Avoid areas where bees are present, such as flower gardens, orchards, or fields with blooming plants. Wear protective clothing, including long sleeves and pants, when engaging in outdoor activities that might disturb bee colonies. If you must work or walk through areas with high bee activity, try to do so during cooler parts of the day (usually early morning or late evening) when bees are less active.
Remember that some medications and treatments can also increase your sensitivity to pollen. Consult your doctor about potential interactions before undergoing any new therapy. By making these simple adjustments, you can significantly reduce your exposure to bee pollen and alleviate symptoms associated with an allergy.
Treatment Options for Severe Reactions
If you experience severe reactions to bee pollen, it’s crucial to seek immediate medical attention. In such cases, doctors may prescribe epinephrine auto-injectors like EpiPen to help alleviate symptoms. These devices can be life-saving during anaphylaxis attacks, which often manifest within minutes of exposure.
Antihistamines and corticosteroids are also used in treating severe reactions, although their effectiveness may vary from person to person. Allergists may recommend a combination of medications for managing allergic responses, including antacids to neutralize stomach acid and prevent further complications.
In more severe cases, patients might be hospitalized for close monitoring and treatment with intravenous corticosteroids or immunoglobulin therapy. In some instances, oral desensitization therapy (ODT) may be recommended by doctors as an alternative to traditional allergy treatments. This involves gradual exposure to small amounts of the allergen in a controlled environment.
Always consult your healthcare provider before attempting any new treatments or therapies. Keep emergency contact information readily available and make sure you have access to medication at all times, especially during peak pollen seasons.
Frequently Asked Questions
What if I have a mild bee pollen allergy, can I still take supplements or eat foods that contain bee pollen?
While it’s essential to be cautious, some people with mild allergies may still choose to consume bee pollen products or foods containing bee pollen. However, it’s crucial to consult a healthcare professional before doing so and follow their advice carefully.
How do I know if my symptoms are caused by a bee pollen allergy or another underlying condition?
Symptoms of a bee pollen allergy can be similar to those experienced with other allergies or conditions. To determine the cause of your symptoms, work closely with your healthcare provider to diagnose and rule out other possible causes through a combination of medical history, physical examination, and diagnostic tests.
Can I be allergic to both bee pollen and other types of pollen?
Yes. Cross-reactivity between different types of pollen is common due to their similar protein structures. If you’re allergic to one type of pollen, it’s possible that you may also react to others, including bee pollen.
How can I minimize my risk of exposure to bee pollen in everyday life?
You can take steps to reduce your exposure by avoiding areas where bees are active (e.g., flower fields), wearing protective clothing when outdoors, and checking food labels for bee pollen content before consuming them. Additionally, inform others about your allergy to ensure they take necessary precautions around you.
What should I do if I experience a severe reaction or anaphylaxis due to a bee pollen allergy?
In the event of a severe allergic reaction or anaphylaxis, call emergency services immediately and administer epinephrine if available. Keep in mind that prevention is key; consider consulting with your healthcare provider about developing a personalized action plan for managing your condition and minimizing future risks.
